Telemedicine Web & Mobile App development: Cost and Process
By reading this article, you will get a complete picture of the best solutions for developing telemedicine applications. In this article, we will try to describe in detail the processes of telemedicine software development and also will tell you how to start your project.
You will find out:
1. Telehealth service delivery models:
- Real-Time Telemedicine
- Store-and-Forward Telemedicine
- Remote Patient Monitoring
- mHealth
2. The core components of telemedicine software for patients.
3. The core components of telemedicine software for doctors
4. Regulatory approaches to telemedicine
5. Deployment: Web & Mobile application architectures
6. Stages of telemedicine software development process
7. How much does it cost to develop telemedicine applications?
Telehealth service delivery models
The concept of remote health care isn’t new, but it’s become more widespread due to providing access to the software and tools required to connect physicians and patients remotely. All types of telemedicine solutions existing in the world today are conventionally classified into four categories: real-time, store-and-forward, remote patient monitoring (RPM), mHealth.

Real-Time Telemedicine
During a real-time telemedicine encounter, patients and providers use video conferencing software to hear and see each other. Video conferencing is approved for primary care, urgent care, follow-up visits, and the management of medications and chronic diseases. It is important to note, that the consumer video communication applications that we use to connect with friends and co-workers, like Zoom and Skype, are not appropriate for telemedicine. Real-Time telemedicine requires video conferencing or audio telecommunication platforms that are HIPAA compliant.
Examples:
- Stroke telemedicine (or telestroke) consultations for neurologists to assess patient symptoms;
- Live remote pediatric specialist consultations;
- Mental health and psychiatric assessment.
Store-and-Forward Telemedicine
Store-and-forward telemedicine, also called asynchronous, is the opposite of real-time telemedicine. It allows patient health and medical data to be collected and then securely transferred to a secure cloud-based platform that other authorized users can then access at any time. Store-and-forward telemedicine is an efficient way for patients, primary care providers, and specialists to collaborate because they can all review the information when it is convenient for them. It uses a solution that has built-in advanced security features to ensure patient confidentiality. This type of telemedicine is especially used for diagnostics and treatment in dermatology, ophthalmology, and radiology.
Examples:
- Radiology x-rays or MRIs reviewed by remote physicians;
- Digital photos of skin conditions reviewed and treated remotely if needed in dermatology;
- Remote testing in pathology;
- Remote eye screenings for diabetic retinopathy in ophthalmology;
- Patient portals allow communication between a patient and their GP.
Remote Patient Monitoring
Remote patient monitoring (RPM), also known as self-monitoring or telemonitoring, uses a range of technological devices to remotely monitor a patient's health and clinical signs. This type of monitoring is often used to manage high-risk patients and patients with chronic diseases (diabetes, hypertension, etc.). During a pandemic, RPM solutions allow chronically ill, at-risk and recovering patients to stay home instead of being in a hospital or clinic.
Examples:
- Remote care management of chronic diseases;
- Implantable or patient-controlled remote monitoring devices for heart failure;
- Glucose trackers for patients with diabetes;
- Remote monitoring for long-term and post-acute care;
- Remote monitoring based on care coordination programs;
mHealth
mHealth is a form of telemedicine that involves providing clinical and medical services through smartphones and other wireless and mobile devices. It is common practice to use individual medical devices connected to smartphones or tablets, “smart” boxes for pills that notify patients if they forget to take their medication, and various mobile medical applications.
Examples:
- Physician downloads photos of a patient’s dermatologic condition to provide diagnosis and treatment;
- The diabetic patient connects a glucometer to his smartphone to track and transmit data to the clinician;
- The provider conducts face-to-face or electronic medical consultations through a secure healthcare app.
McKinsey Global Institute has determined that doctor-to-Patient telemedicine consultation platforms are the most capacitive segment now, covering more than 48% of the market.
In addition, the COVID-19 pandemic has had a major impact on the growth of the telemedicine market. States are using social distance and isolation tactics to reduce the spread of the virus. As a result, some patients cannot access medical care in person. Thus, the number of teleconsultations is increasing. As more and more people use telemedicine, this will stimulate market expansion.
The core components of telemedicine software for patients
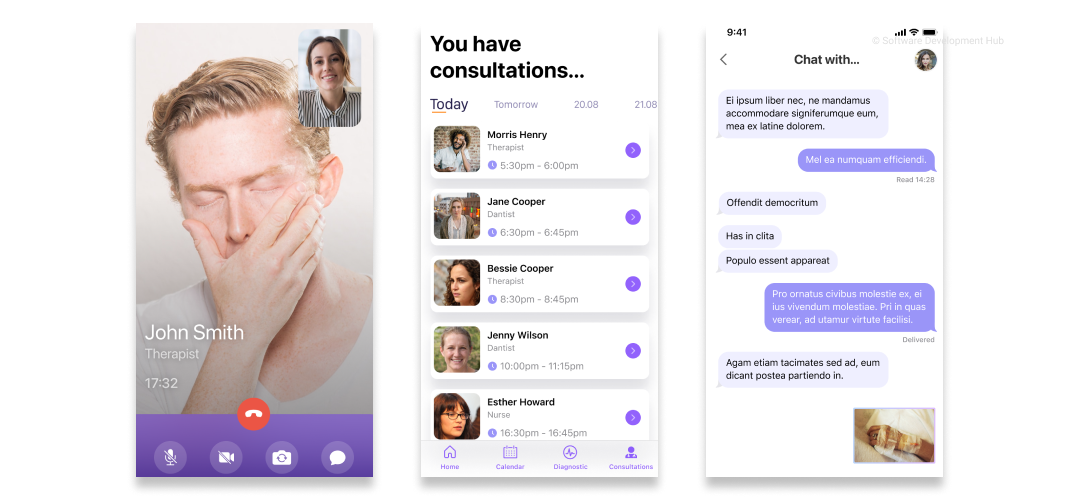
When creating a patient-centric application, you should study in detail the business logic of remote medical care. The mHealth applications allow patients to get first aid when they need it. More importantly, patients can communicate face-to-face with a specialist through video chat and live conferences. It is already routinely used in medical and diagnostic practice.
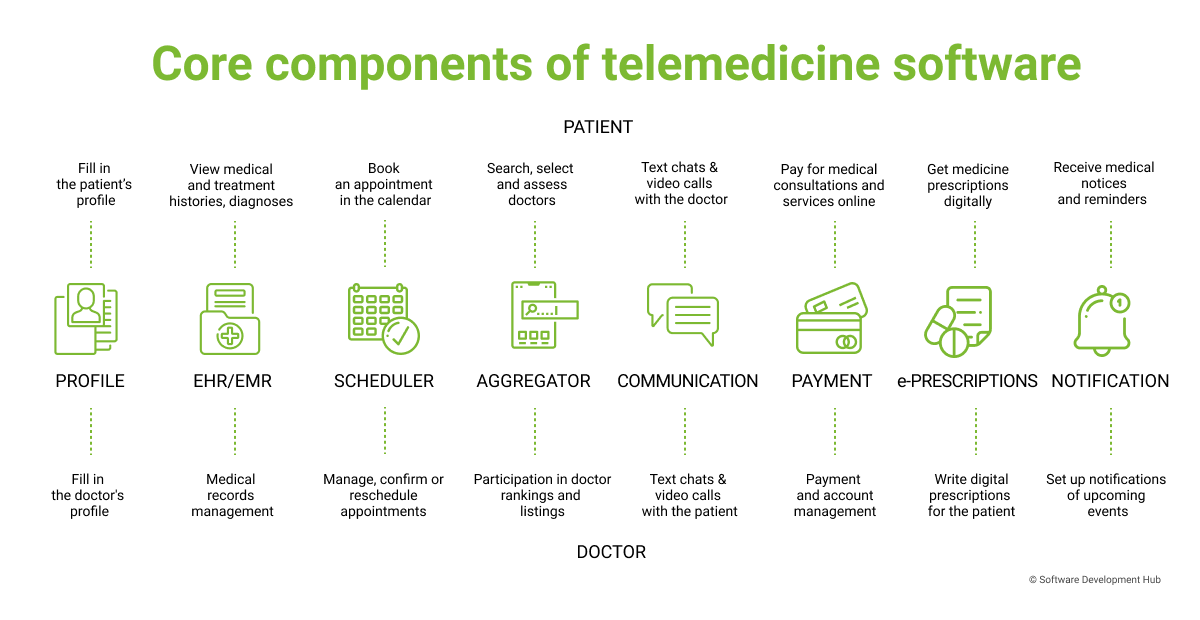
Patient-related features:
- Registration. Patients can register by phone, social networks, or email. Since the application works with confidential data, it requires a higher level of personal data protection. It is recommended to use two-factor authentication, which may include SMS, voice, and telephone verification.
- Patient profile. The patient indicates his contact details and other data and creates an electronic medical record. Creating a patient profile should be as simple as possible so that even an inexperienced user can easily specify his data.
- Search — the patient can search for a medical professional by one or more criteria (specialization, geolocation, doctor rating, etc.).
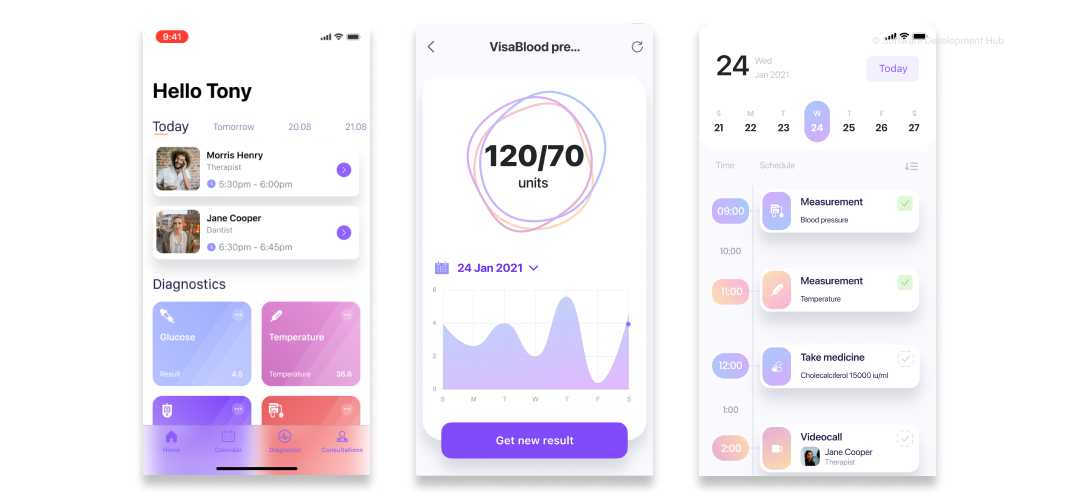
- Appointments and calendar. The name speaks for itself: a telehealth platform should provide booking appointments and managing schedules for maximal efficiency. Patient-driven appointment requests help to choose a timeslot for any physician of their choice on the day and time that best fits their availability.
- Electronic health records (EHRs) or electronic medical records (EMRs) are digital version of paper charts. History of medical referrals, diagnoses, tests, and treatments are usually available on electronic health records.
- Communication. The process is performed through audio or video communication for real-time consultation. For the first version of telemedicine applications development, it is reasonable to implement a simpler option — text and/or photo chat. There are certain standards for the transmission, storage, and interpretation of medical pictures and images recorded by digital media, which have some differences in different countries. In the healthcare sector, it is crucial to use end-to-end encrypted messaging protocols to protect communications and prevent attacks.
- Payment. To monetize telemedicine services, it is necessary to integrate the payment gateway system into the application. The patient should also be able to view the history of his finance operations.
- Notifications. Push notifications and corresponding reminders help to follow the assigned consultations.
- Ratings and reviews. This feature is necessary if you have a “doctor-to-patient” aggregator.
In developing telemedicine applications for patients, it is important to consider user experience and the relevance of the options offered. The patient application may also include some additional features, for example:
- Drug tracking. The application can remind the patient to take the necessary drugs.
- Patient insurance plan. This is a useful feature for integrating with insurance companies and providers.
- Sick leave. If the doctor issues a sick leave, the patient can send it to his employer directly through the application.
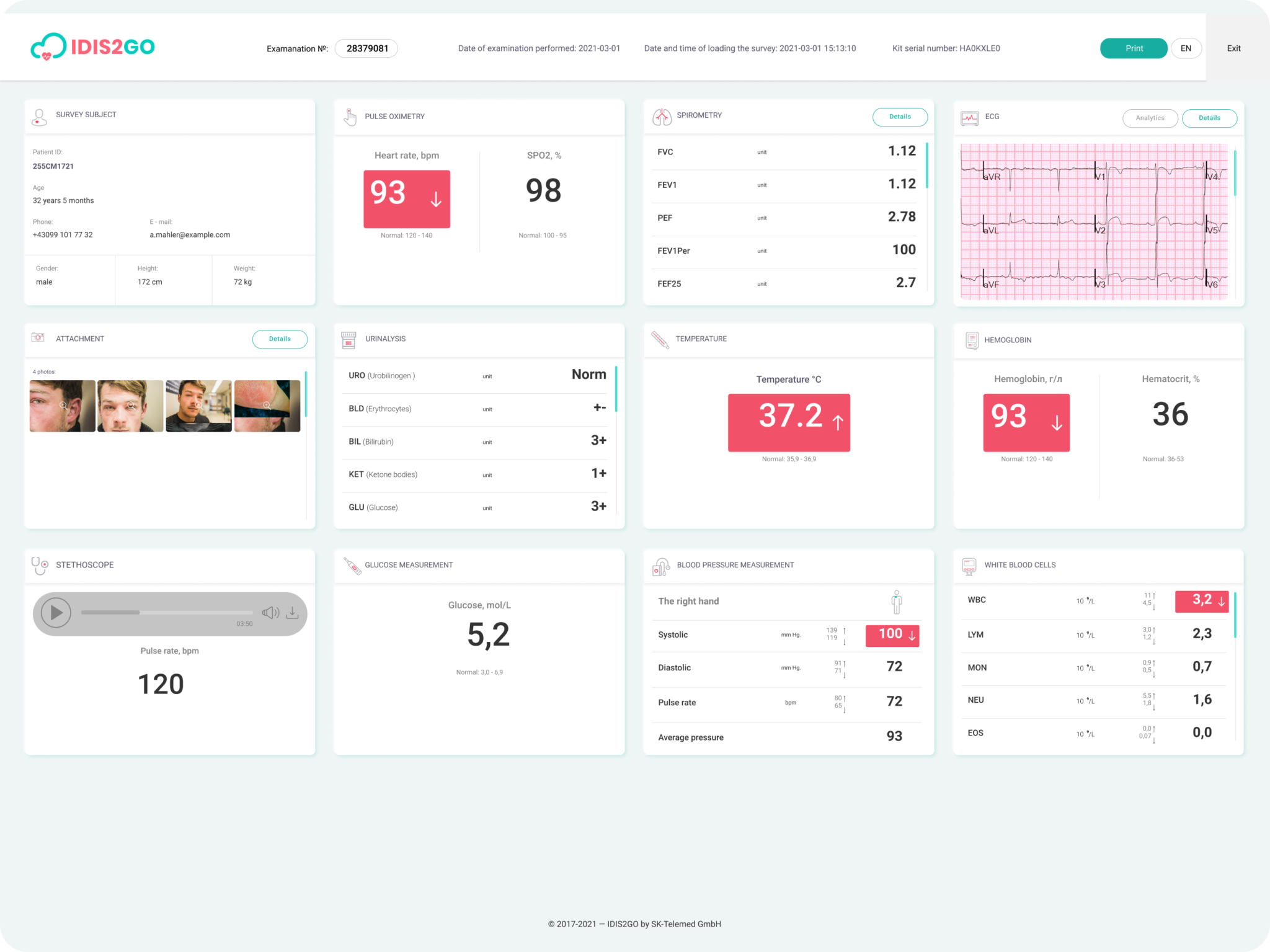
- Integration with home telemetry devices. Through the application, you can send reports from connected devices directly to the patient’s medical records so that the doctor is analyzed. Using IoMT technology and AI algorithms, the telemedicine application facilitates health monitoring and offers suitable treatment solutions.
- Daily monitoring log. The telemedicine solution offers daily symptom monitoring if the patient is undergoing outpatient treatment with COVID-19 or is self-isolated. For example, the monitoring schedule includes temperature and respiratory function measurements. A patient can be tested at home using self-monitoring devices without the need to be hospitalized. A physician can remotely monitor changes in symptoms and respond immediately to the deterioration of the condition. Such projects are already being implemented all over the world. Thus, the labor costs for patient care are reduced, and the number of severe cases is decreased.

The core components of telemedicine software for doctors
The telemedicine software solution for doctors and clinics helps optimize the main processes handled in the clinic from patient record management to scheduling and workflow management. As for the telemedicine application for physicians, some functionality correlates with the patient software.
Doctor-related features:
- Doctor profiles, where doctors fill in accurate information about their specialization, experience, education, etc. It is possible that patients may want to check their license and proof of medical ability or working hours.
- Patients. The doctor can see a list of patients he treats or consults with within the telemedicine platform. By clicking on any patient, a user is redirected to the patient page where you can find all the information about the patient such as name, visit history, notes and records, tests, etc.
- Scheduling and appointments. The COVID-19 pandemic is making healthcare facilities burst from their seams. In situations that demand a high volume of patient bookings, the ability to plan and schedule appointments becomes critical.It is necessary to have a visit scheduler or calendar with events. The calendar keeps the doctor informed about meetings and the latest events. It helps to see who is booked and at what time. Doctors can manage appointments, and confirm or reschedule appointment requests.
- EHRs (as opposed to EMRs) are designed to be shared with other providers, so authorized users may instantly access a patient’s EHR from across different healthcare providers. It is a must-have feature that automatically sends physician notes to electronic EHR-records to avoid duplication of work.
- Communication. Doctors can connect through in-app chat, in-app calls, or video sessions. In the early versions of the product, it is good to start with text chats or photos-based consultations. With a larger budget, it is better to use video conferencing modules that help the doctor diagnose the patient using visual clues. It elevates the quality of diagnosis as the doctor can visually examine the patient, take note of their voice, and communicate the treatment effectively.
- e-Prescriptions. For prescribing the medicines to patients digitally. The patient can then get prescriptions from the pharmacy or the required medical service.
- Reports and Analysis. Data analysis and reporting is more of a pleasant(peasant) полезная feature for healthcare establishments that want to monitor their performance, number of patients, revenue fluctuations, etc.
Other useful features that can be included in the telemedicine application for physicians:
- Pharmacy databases. It includes up-to-date medication listings by the following categories: pharmaceutical formulation, license, trade name, composition, etc. This feature also may become a module integrated into the medical information system for doctors and clinics use in general. You can see our case Medicine Registry.
- Medical equipment integration. With the help of IoMT, technology doctors can get instant access to the results of clinical trials and diagnostics. These solutions help collect patient data from different medical devices and store them in one place so that doctors can provide appropriate treatment based on information stored in a single EMR system. IoMT is a critical piece of the digital transformation of healthcare, as it allows new business models to emerge and enables changes in work processes, productivity improvements, cost containment, and enhanced customer experiences.
- Automated performance dashboards. Embedding configurable clinical and administrative reporting tools into an enterprise telehealth platform with import and export connections enables consistent access to real-time dashboards and reporting services.
Regulatory approaches to telemedicine
If you want to create an application in health care, including telemedicine, you should consider the legal framework of the country where it will work. Each country has its own legal requirements that your telemedicine product must meet.
For example, the U.S. has HIPAA (Health Insurance Portability and Accountability Act). The U.S. Telemedicine Association has conducted extensive research and created guidelines addressing clinical, administrative, and technical issues.
The regulatory framework of the European Union on telemedicine is not yet fully developed. In addition to Directive 2011/24/EU, Directive 95/46/EU, Directive 2000/31/EC, and Directive 2002/58/EC, GDPR (General Data Protection Regulation) remained the most important standards today.
The regulatory framework and policy should always be your focus in developing telemedicine software.
Deployment: Web & Mobile application architectures
75% of the respondents preferred telemedicine software accessible through a web browser on a PC or Smartphone. This feature was popular because most hospitals and clinics didn’t prefer installed software that is hard to maintain.
Moreover, browser-based web applications are easy to distribute and can be accessed by anyone with minimum friction. There are no specific system requirements or lengthy update procedures that hinder the usability of the software. Hence, telemedicine web applications should be an important checkbox on your priority list.
Patients, of course, prefer mobile applications. Depending on your target audience, you should choose to develop a native application for iOS or Android.
Stages of telemedicine software development process
Discovery stage
1. Idea and Research (business analysis stage)
At this stage, business analysts take your idea and turn it into an action plan that can be used as the basis for a future telemedicine application. At this stage, market and competitor analysis is conducted to accurately design the system.
Telemedicine project business model canvas — Example
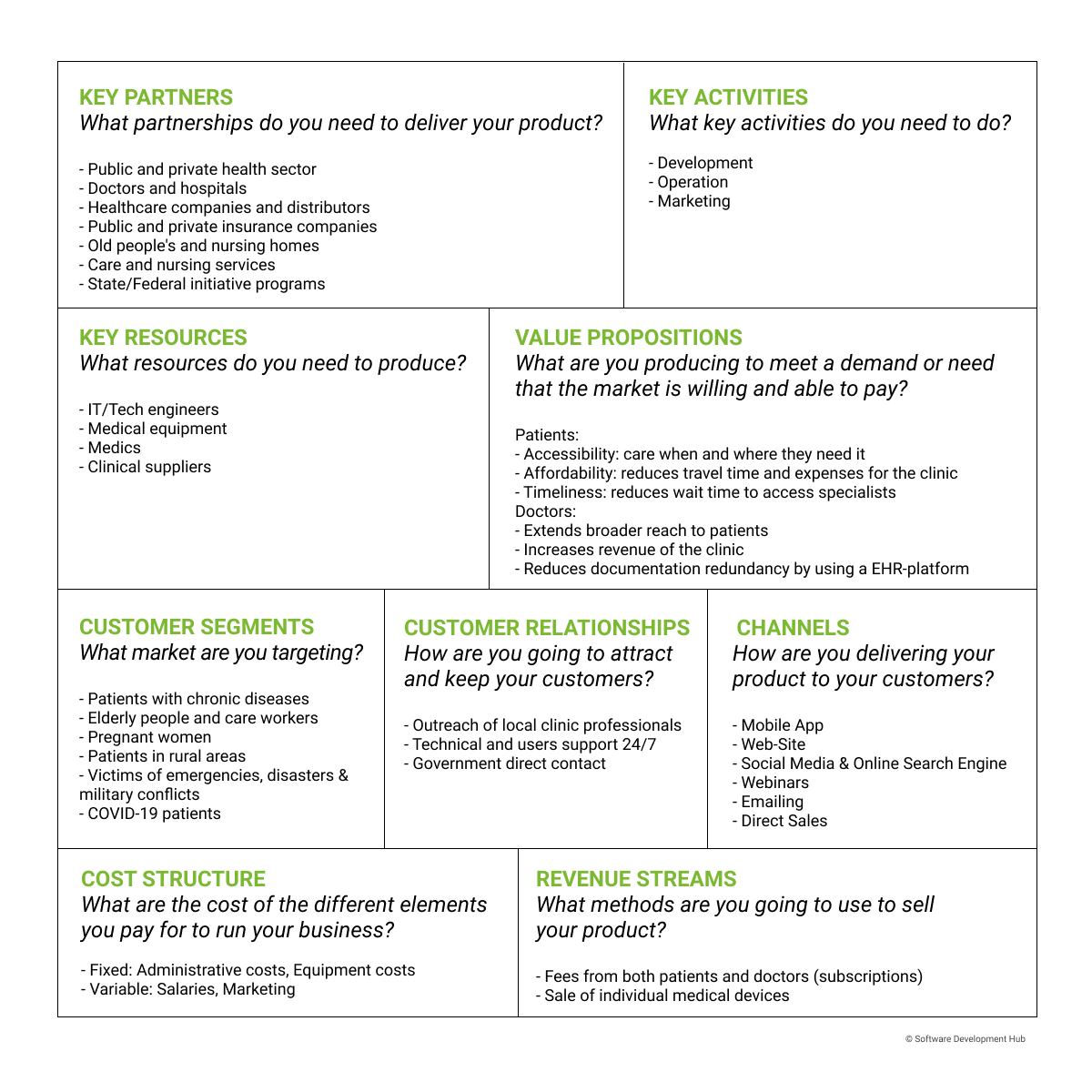
The preliminary plan can be as follows:
- Identify the exact target audience
- Define the application’s purpose
- Develop a business plan for the project (including income)
- Create reliable application content and organize data
- Budget planning for telemedicine application development and marketing costs
- Product design and implementation with a team of professional software developers.
The target audience for telemedicine may include medical service providers, public health institutions, patients, healthcare professionals, healthcare organizations, and so on. The type of project you choose will affect the process of developing telemedicine software.
2. Design.
UI/UX designers use business analysis results to create an attractive system interface. UI/UX takes into account the specific interaction of both user groups — doctors and patients.
- Since Software Development Hub has successfully implemented several major telehealth projects (IDIS, Telemed24, RMDS app), we are ready to provide you with an example of a proposal for the Discovery stage, which combines the stages of business analysis and design into one package of all the basics necessary to further develop a successful telemedicine product. In addition, it contains cost estimates.
Development stage
- 3. Software development (coding)
At this stage, various software development specialists (back-end, front-end, Android or iOS developers, full-stack developers) are involved under the supervision of the project manager. Fortunately, they will have a solid foundation and accurate plans from the previous stages.
- 4. Quality assurance and UAT testing
Debugging and testing telemedicine software is the process of working with the program on test examples to find and eliminate errors in the program. QA specialists must come to the conclusion that the product is error-free and ready for release.
- 5. Support and maintenance
Once a telemedicine solution is deployed, it must be updated and maintained to remain reliable and productive, regardless of circumstances.
Following the release of the telemedicine application, it must be updated and maintained so that it remains stable and up-to-date, regardless of the circumstances.
How much does it cost to develop telemedicine applications?
Unfortunately, we will not be able to give the exact cost of creating a telemedicine application. The price range depends on the nuances of the development and functional features of particular software.
It is necessary to estimate the cost of developing the telemedicine platform itself and allocate a budget for the promotion and distribution of the application.
The discovery phase is especially useful if you want to determine the cost of a startup in telemedicine because it will also give you visible results that can be used to attract new investors. For example, the discovery phase, in addition to providing a cost estimate, depending on the selected package, will give you:
- product concept from the product manager
- business intelligence prototypes
- the visual concept from UI/UX designer
- architectural concept.
The cost of developing a telemedicine application largely depends on its concept, functionality, development approach, and the selected developer. When working with an offshore agency for the development of mobile applications, you can count on the fact that the first working version for one platform (iOS, Android or Web) will be spent about $60 000 – $100 000.
If you want to add more functionality or create an application of greater complexity, be prepared to spend more money.
| Task/features | Time for development, h | Approx. cost, $ |
| Pre-development activities: planning of an application structure, finalizing requirements, server setup, continuous integration, etc. | ~100 | 5,500 |
|
Core features development:
|
~160-300 | 25,000 – 30,000 |
|
Additional features development:
|
~100-180 | 9,000 – 15,000 |
Please note that this price includes the application for the patient, the application for the doctor, and the administration panel for one platform (iOS or Android), the hourly rate of 25-40 dollars. The terms of development vary from about 4 to 6 months.
Categories
Share
Need a project estimate?
Drop us a line, and we provide you with a qualified consultation.